I've been incredibly touched by all the comments on the last couple of posts, and by the texts, emails and phone calls expressing so much empathy, support and encouragement. It feels wrong not to reply to them all individually to say how much I appreciate them, but they've really made a difference: it makes me feel much less alone. Thank you so much.
I spent a fair amount of time this last week gearing myself up for seeing the consultant, Professor Cunningham (I'd asked to see him in person this time, although I've only met him once, very briefly, just before I started treatment back in November 2010). I marshalled all my arguments as to why they shouldn't give up on treating me; I looked up all the drugs the surgeon in Frankfurt had used (always a cocktail of three or four, with the main two staying the same but alternating the use of several others) which had seemed effective in controlling the tumours and which I could ask them to try now; I researched bile duct cancer (which is what they think the most likely source of my primary tumour) and made a list of all the drugs used to treat it so that I could counter any argument that "there are no other established treatments"; I talked with various people about how much right I have to insist on any particular treatment, and how best to go about making it a constructive conversation.
Then the day before the appointment I was phoned by the doctor I'd seen at the beginning of the week, who told me she'd discussed my case with the consultant, and he'd decided to carry on with the current chemo but replacing the tablets with the intravenous version. The plan is to do another three cycles - providing I can tolerate it OK - and then do another scan. This will provide a comparison with the recent scan, and give a clearer idea of whether these drugs are effective or not. She'd made me appointments for next week (blood tests on Monday, then chemo on Wednesday), and suggested cancelling the appointment with the consultant since he would simply repeat what she was telling me. I agreed that the plan makes sense, and that there seemed little point in keeping the appointment.
I must admit that I'm nervous about continuing: although I hope that the intravenous version of the second drug will avoid some of the unpleasant side-effects on my guts, I'm not yet sure how easy it will be to manage being attached to a chemo pump for two days. The cycle will be once every two weeks instead of every three, so it means less recovery time between doses, and after having a week off and feeling considerably better for it, it's daunting to go back into treatments which have left me feeling so washed out. All the same, this is certainly what I was hoping for - I'm very glad that they're prepared to take a bit more time to assess the efficacy of these drugs, and I'm extremely relieved to have the structure of treatment for a few more weeks. So I'm happy with the new plan.
What's been interesting is that alongside the relief has been an element of anti-climax in being told, essentially, that we're back to business as usual, after such a challenging week emotionally. I had some flashes of anger with the doctor who'd told me that I might have reached the end of the road at the Marsden, and for having gone through all that fear about this being the beginning of the end, when perhaps it wasn't strictly necessary. (Although I imagine that this will be a conversation which will happen sooner or later - maybe in 6 weeks' time at the next review - so I'm sure my research and preparation haven't been wasted.)
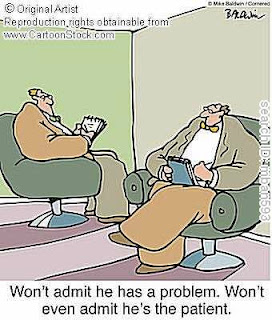
But I think the main reason for my annoyance is that this has highlighted a low-level but ongoing frustration with my medical team: feeling that my views aren't really taken into account. A friend recently reflected how my default position is to challenge my doctors, to argue with them, to assume that I need to work hard to get across my wishes and opinions. She's right: I'm not always as bolshy as that might imply! but it's true that I don't take for granted that I can trust them to know what's really best for me. Part of this, I'm well aware, is my own emotional pattern: fearing that if I don't shout loudly enough I'll be overlooked, or dismissed as unimportant, or forgotten about, or not really thought about carefully (of course, in true psycho-babble cliché, these are all variations on fears of being abandoned). Added to that, I'm also aware that I find it very hard not feeling in control, and that wanting to debate and challenge my doctors is partly about not fully accepting being in a patient role.
However, the model of care at the Marsden also plays a part in this dynamic. I have no doubt that all the doctors there - from consultants to registrars to junior doctors - are extremely expert and competent, and the nurses in the chemo unit are without exception pleasant and friendly as well as skilled. What's lacking is any continuity of interaction; any sense of anyone getting to know me; any reassurance that somebody is holding in mind the bigger picture of me and my treatment journey, rather than just the part that they're doing today and which someone else will do next time.
I've rarely seen any doctor more than once (the maximum was three times, twice of which was on consecutive days' ward rounds when I was in hospital in June 2011, and the third time by chance in clinic later), and I must have seen at least two dozen different doctors over two years. All are efficient and knowledgeable - they check for side-effects before each chemo session, and at each review appointment they feed back to me my scan results, or whatever decision has been made in their team meetings - but no one person knows anything about me except what's in my notes and whatever the scans and blood tests show, along with the report of whoever saw me for the most recent 10-minute consultation. The consultant I'm under has ultimate responsibility for me, and I don't doubt that his decisions about my treatment are based on vast clinical experience, but he wouldn't recognise me if he saw me, nor I him.
Of course I realise that every patient can't see the consultant every time, but the lack of any consistent contact with one - even relatively junior - doctor who knows me leaves me feeling as if decisions are made solely on technical data about the inside of my body, without any interest in my thoughts or opinions as a whole person living with a life-limiting illness. It's not that I believe being a "case" rather than a "person" compromises the effectiveness of the treatment prescribed; it's simply that the process feels pretty impersonal. I have no doubt that I respond to all this (often in a knee-jerk way, and not always helpfully) by arguing or discussing or asking detailed questions, not only for the actual information but also in order to feel noticed, to make sure I'm taken seriously, and to reassure (or convince) myself that I, Sylvia, am actually involved in this process and not simply a passive diseased body.
There was one notable exception - the registrar who I saw at my first appointment at the Marsden after being referred on from Chelsea & Westminster, where I was diagnosed. I saw him for the second time on the day of my first chemo, when I was feeling extremely scared and vulnerable and overwhelmed (though, typically, trying hard not to show it), and I remember he took both my hands and said to me, "don't worry, we're going to take great care of you". I was hugely warmed and comforted by that, and thought how glad I was that he was my doctor. Oh, how naïve: I never saw him again - presumably his rotation ended soon afterwards. Since then, many doctors I've seen have taken lots of trouble to provide "good care" - e.g. making copies of reports for me, accessing super-detailed results I've asked for, answering my endless questions - but it's all been with professional efficiency rather than warmth. "Care" is very different from being cared about... Similarly, several of the nurses recognise me by name, and some remember that I used to go to Germany, but it's a big unit with a lot of staff, and I'm generally attended to by different nurses each time I go for chemo.
I appreciate that this sounds very critical, and perhaps ungrateful and unfair. I'm aware that the Marsden is renowned as one of the top cancer hospitals in the world, and that I'm incredibly lucky to have free high-quality medical care there. In my defence, perhaps I feel especially strongly about this issue because of having worked for six years in a medical setting as a psychologist, and therefore having thought a great deal about patients' experiences of medical systems.
Certainly at work I had differences of opinion at times with my doctor colleagues (who are trained to think in a very different way from psychologists), but I always hugely admired and respected their attention to building collaborative relationships with their patients. Naturally, for psychologists, establishing a good relationship with clients is the most important thing, so of course I'm biased, but part of what I liked about HIV medicine was how it was readily acknowledged that people's emotions and ways of seeing the world, and how they relate to doctors and to their condition, have to be taken into account, and taken seriously. Those factors affect whether patients can tell partners or family about their HIV status, whether they use condoms or not, whether they blame themselves if they become unwell, whether they take their medication or avoid it because it's a reminder of HIV - and whether they admit any of this to their doctor. So doctors need to get to know their patients, to understand what their fears and concerns are, to build trust that they'll be listened to and not judged, so that patients know their treatment is being done with them, not to them. The clinic was designed so that patients always saw the same doctor (unless they requested a change, or for emergency appointments), sometimes for decades; and this meant that doctors supported their patients through all the milestones of diagnosis, starting antiretroviral therapy, treatment changes and treatment failures, episodes of illness or crisis, as well as significant life changes unconnected to HIV. I was very heartened to see how effectively the doctors embraced this principle of treating patients as people, and how much that enhanced patients' experiences of their treatment (and sometimes other areas of their lives too).
If I was convinced of this when I was a healthcare professional, when I became a patient it was strongly reinforced by my experience at the German clinic, where I saw Dr Herzog two or three times every visit, so I got to know him, and he got to know me, quite well over my year of treatment there. It meant a huge amount to me that not only could he remember my medical history without looking at my notes, but he also knew I play the violin, and find irreverent humour funny, and wanted reassurance that I was doing enough alternative treatments, and longed to go skiing, and needed to be given permission (or ordered!) to relax. It made a huge difference to how supported I felt and how much trust I had in him, and it seems a shame that this isn't better acknowledged at the Marsden.
I appreciate that it's a big teaching and research hospital, where staff presumably have fantastic training by being able to move around departments frequently, and that this increases their skills and competencies; but the downside for patients is not seeing the same doctor throughout even one course of treatment (assuming that my experience isn't unusual). Similarly, a specialist nurse told me that their weekly team meetings involve up to 50 clinicians from different disciplines (oncology, radiology, surgery, academia etc), so they draw on a huge wealth of expertise; but almost all those present will be talking about patients they've never met and never will. It's ironic, and sad, and frustrating, that many of the Marsden's sources of "excellence" actually create what can feel like a fragmented, authoritarian and impersonal system.
I'm sorry for indulging in a bit of a rant. Overall the Marsden's done very well in looking after me, and I'm aware it's not their fault I have cancer and have to lead a life I don't really want - perhaps I just needed to let off a bit of steam, and they're an easy target. I know I can't attribute my confrontational attitude solely to everyone else's shortcomings, tempting as it is - it can't be easy to deal with sceptical control-freak argumentative patients like me! (even though I also try very hard to be liked, which must balance things out a bit) - but I'm pretty sure their system doesn't massively help foster trust either.
So you can see why, although I was very relieved to be spared yet another trip to the Marsden, and although I'm suitably grateful to have a treatment plan sorted out for me, I also felt a bit deprived of the chance to actually talk to the man at the top who has so much influence over my life. (Not God, the other one.) I guess I'll have to leave it for another time - but as you'll have gathered, he definitely hasn't heard the last of me!

I can really see the loss in being a patient whose local practice and specialist nurse is the Marsden, rather than aDGH whe you would certainly see a less 'expert' team, but what you would get is one who have fewer patients and are therefore better able to be alongside you, Sylvia, in your experience, progresas and treatment.
ReplyDeleteBtw, Humph, Kate, Clare and Barbara send their love to you xxx
I'm sure many people can relate to the 'patient' experiences you discuss here so well. I think you handle yourself brilliantly and should never apologise for wanting to be in charge of your own destiny. When it comes down to it you're one fiesty gal! x
ReplyDeleteAn interesting rant, Sylvia. From the sound of it the Marsden should stick a barcode on each patient, as it seems as though you are as significant as a sack of potatoes in Tesco's! From a practical point of view, having 50 clinicians discussing cases in a meeting is a hugely inefficient waste of resources. I've recently had a string of meetings with up to 27 attendees, and even that number is beyond what is practical for a productive gathering.
ReplyDeleteThe constant 'churn' of staff involved in your case (I hesitate to use the word 'care') is similarly inefficient in that your notes have to be read and re-read numerous times - and the notes themselves take time to be written in the first place! There's also an element of Chinese whispers which could lead to misinterpretation of what's been written.
On the plus side, the purpose of the Marsden is to obtain the best clinical outcomes for the patients. Maybe it's better that the tea and sympathy is left to friends, family and social workers, leaving the medical expertise to focus on keeping the cancer at bay - even if makes you feel like you're on the vegetable rack in Tesco!
The combination of Dr Herzog and the Marsden's fabulous fifty have done you well, so thumbs up to them, and to you, in getting this far in spite of the facelessness and disorganisation that gets you frustrated from time to time. It was never going to be easy, so keep up the good work and keep smiling.
Ah, deem not that this simple little flower
ReplyDeleteUnfolded all its tender bloom in vain;
Did it not glorify a summer hour,
And leave a sweetness in the summer rain?